SCIENCE OF IBS
IBS has many contributing factors
IBS is a disorder of the brain-gut axis and has long been considered to have a multifactorial pathophysiology, with a complex array of contributing factors1-4
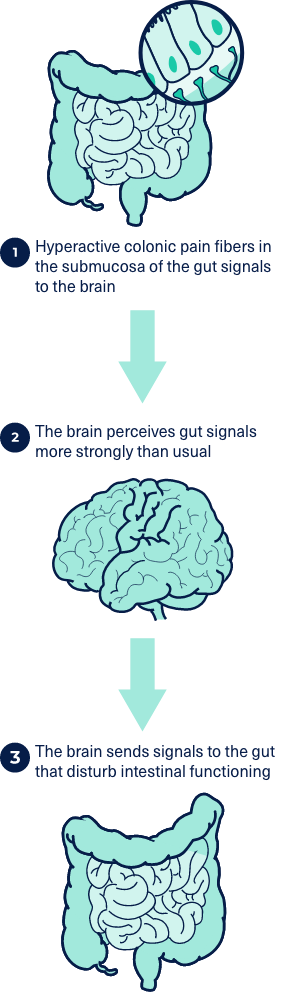
The Mechanism for Abdominal Pain in IBS5-7
VISCERAL HYPERSENSITIVITY AND ALTERED CORTICAL PERCEPTION IN IBS5-7
IBS is thought to be associated with visceral hypersensitivity and pain caused by hyperactivity of colonic pain fibers located in the submucosa of the gut. These fibers signal to the pain-sensing regions of the brain, causing a disconnect between brain-gut communication that results in the brain perceiving gut signals more strongly than usual and sending signals to the gut that disturb intestinal functioning.5-7
IBS TRIGGERS
The visceral hypersensitivity, altered cortical perception, and abnormal gut motility associated with IBS can be triggered by numerous other factors, including certain foods, chronic stress, lack of sleep, menstrual cycle, and pregnancy.1-4
ROME IV IBS CRITERIA8
Recurrent abdominal pain at least 1 day per week, on average, associated with 2 or more of the following criteria:*
- Related to defecation
- Associated with a change in frequency of stool
- Associated with a change in form (appearance) of stool
Rome Clinical Considerations
The Rome Foundation suggests for clinical practice, a diagnosis may be made with a lower symptom frequency and a shorter duration (8 weeks or more) than those required above, provided that symptoms are bothersome for the patient (i.e., interfering with daily activities/quality of life) and there is clinical confidence that other diagnoses have been sufficiently ruled out.
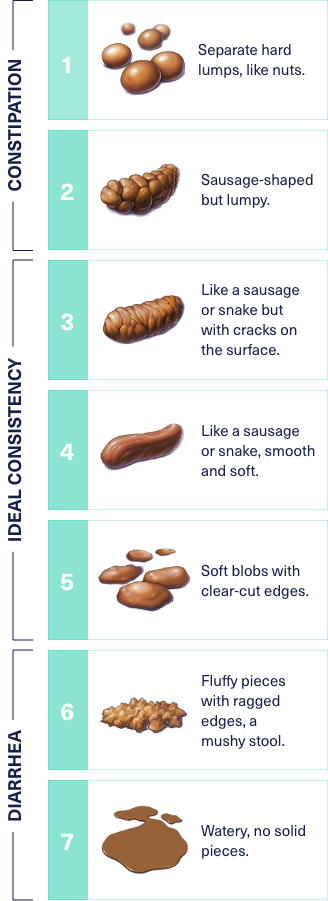
ROME IV IBS-C SUBTYPE CRITERIA8
- Abdominal pain related to defecation
- >25% Bristol stool type 1 or 2
- <25% Bristol stool type 6 or 7
ROME IV IBS-D SUBTYPE CRITERIA8
- Abdominal pain related to defecation
- >25% Bristol stool type 6 or 7
- <25% Bristol stool type 1 or 2
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis.
Downloadable Resources for You and Your Patients
An open dialogue focused on understanding the patient’s most bothersome symptoms may help reduce treatment delays and improve treatment expectations. The resources here are designed to help start the conversation and help with patient education and treatment management.